
Hemorrhoidectomy remains the "gold standard" of treatment. With this understanding, it may be offered to patients seeking a less painful alternative to conventional surgery. Stapled hemorrhoidopexy has unique potential complications and is a less effective cure compared with hemorrhoidectomy. The variability in case selection and reported end points are difficulties in interpreting results. Stapled hemorrhoidopexy has a higher recurrence rate (odds ratio, 3.64 95 percent confidence interval, 1.40-9.47 P = 0.008) at a minimum follow-up of six months.Īlthough stapled hemorrhoidopexy is widely used, the data available on long-term outcomes is limited. Studies in a day-case setting do not prove that stapled hemorrhoidopexy is more feasible than conventional hemorrhoidectomy. The overall incidence of surgical complications was 3.0 (87 cases): anal stenosis (1.8), bleeding (0.8), worsening of anal hypotonia (0.2), sepsis (0.1). Stapled hemorrhoidopexy has a shorter inpatient stay (weighted mean difference, -1.02 days 95 percent confidence interval, -1.47 to -0.57 P = 0.0001), operative time (weighted mean difference, -12.82 minutes 95 percent confidence interval, -22.61 to -3.04 P = 0.01), and return to normal activity (standardized mean difference, -4.03 days 95 percent confidence interval, -6.95 to -1.10 P = 0.007). Qualitative analysis showed that stapled hemorrhoidopexy is less painful compared with hemorrhoidectomy. Follow-up ranged from 6 weeks to 37 months. Meta-analysis was calculated if possible.įifteen trials recruiting 1,077 patients were included. MEDLINE, EMBASE, and Cochrane Library databases were searched using the terms "hemorrhoid*" or "haemorrhoid*" and "stapl*." A list of clinical outcomes was extracted. The specimen should always be sent for pathology examination.This study was designed to determine whether conventional hemorrhoidectomy or stapled hemorrhoidopexy is superior for the management of hemorrhoids.Ī systematic review of all randomized trials comparing conventional hemorrhoidectomy with stapled hemorrhoidopexy was performed.
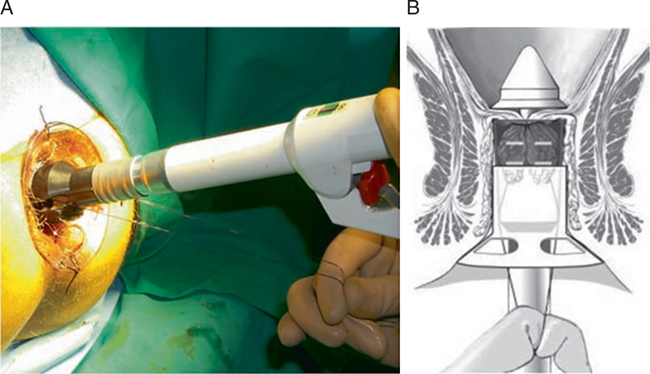
No correlation or differences were observed if smooth muscle was present, although postoperative bleeding was more frequent. Pain was significantly increased if transitional epithelium was present in the specimen. All specimens contained columnar mucosa, but 29.8% contained columnar and transitional epithelium and 12.8% contained columnar, anal transitional, and stratified squamous epithelium. Seven patients experienced pain for a significantly longer period of time. Fissure, skin tags, and anal strictures were observed in 23.4%. Patient's return to work averaged 16.7+/-10.7 days. Immediate complications (first week) were: severe pain in 5.0 of all patients, bleeding (4.2), thrombosis (2.3), urinary retention (1.5), anastomotic dehiscence (0.5), fissure (0.2). Postoperative pain, secretion, and bleeding durations were 12.7+/-10.6, 5.6+/-9.6, and 6.3+/-8.4 days. The risks of stapled hemorrhoidectomy include bleeding, infection, anal fissuring (tearing of the lining of the anal canal), narrowing of the anal or rectal wall due to scarring, persistence of internal or external hemorrhoids, and, rarely, trauma to the rectal wall. Clinical outcome was evaluated by a validated questionnaire. Microscopically, the presence of columnar, transitional, and squamous epithelium, the involvement of circular/longitudinal smooth muscle, and features of mucosal prolapse were assessed. Macroscopic appearance of the specimen (shape, size, and depth) was recorded. From January 2003 to April 2007, 94 patients underwent hemorrhoidopexy. Early and late complications were defined individually with overall data suggesting that. In this prospective audit, we correlated clinical outcome with pathological findings. Overall complication rates of stapled hemorrhoidopexy ranged from 3.3-81 with 5 mortalities documented.
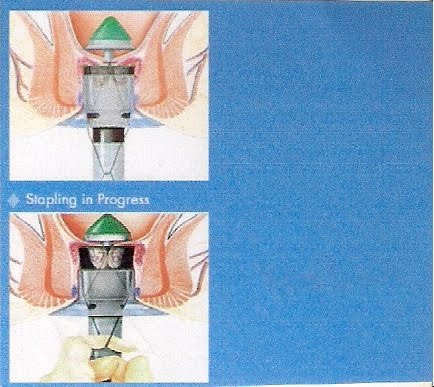
But if it is performed by skilled minimal access surgery the SH is less painful, it was not associated with an earlier return to work than CH, and it failed to deal with external haemorrhoids. Some have been skeptical about this surgery. Stapled hemorrhoidopexy is widely accepted to treat hemorrhoids, but serious complications have been reported. Conclusion: Stapled hemorrhoidectomy is at least as good as conventional haemorrhoidectomy and is less painful.


 0 kommentar(er)
0 kommentar(er)
